Epilepsy (from Ancient Greek ἐπιληψία) is a common and diverse set of chronic neurological disorders characterized by seizures. Some definitions of epilepsy require that seizures be recurrent and unprovoked, but others require only a single seizure combined with brain alterations which increase the chance of future seizures. In many cases a cause cannot be identified, however factors that are associated include brain trauma, strokes, brain cancer, and drug and alcohol misuse among others.
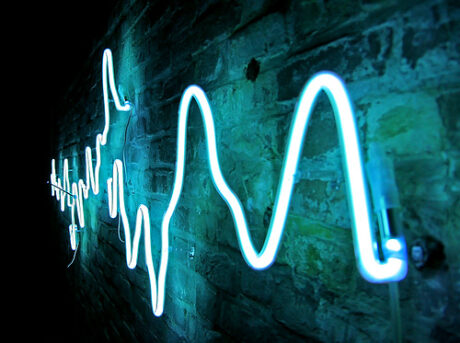
Epileptic seizures result from abnormal, excessive or hyper-synchronous neuronal activity in the brain. About 50 million people worldwide have epilepsy, and nearly 90% of epilepsy occurs in developing countries.
Epilepsy becomes more common as people age. Onset of new cases occurs most frequently in infants and the elderly. As a consequence of brain surgery, epileptic seizures may occur in recovering patients.
Epilepsy is usually controlled, but not cured, with medication. However, over 30% of people with epilepsy do not have seizure control even with the best available medications. Surgery may be considered in difficult cases. Not all epilepsy syndromes are lifelong – some forms are confined to particular stages of childhood. Epilepsy should not be understood as a single disorder, but rather as syndromic with vastly divergent symptoms, all involving episodic abnormal electrical activity in the brain and numerous seizures.
Causes
The diagnosis of epilepsy usually requires that the seizures occur spontaneously. Nevertheless, certain epilepsy syndromes require particular precipitants or triggers for seizures to occur. These are termed reflex epilepsy. For example, patients with primary reading epilepsy have seizures triggered by reading.
Photosensitive epilepsy can be limited to seizures triggered by flashing lights. Other precipitants can trigger an epileptic seizure in patients who otherwise would be susceptible to spontaneous seizures. For example, children with childhood absence epilepsy may be susceptible to hyperventilation. In fact, flashing lights and hyperventilation are activating procedures used in clinical EEG to help trigger seizures to aid diagnosis. Finally, other precipitants can facilitate, rather than obligately trigger, seizures in susceptible individuals. Emotional stress, sleep deprivation, sleep itself, heat stress, alcohol and febrile illness are examples of precipitants cited by patients with epilepsy. Notably, the influence of various precipitants varies with the epilepsy syndrome.
Likewise, the menstrual cycle in women with epilepsy can influence patterns of seizure recurrence. Catamenial epilepsy is the term denoting seizures linked to the menstrual cycle.
There are different causes of epilepsy that are common in certain age groups.
During the neonatal period and early infancy the most common causes include hypoxic ischemic encephalopathy, central nervous system (CNS) infections, trauma, congenital CNS abnormalities, and metabolic disorders.
During late infancy and early childhood, febrile seizures are fairly common. These may be caused by many different things, some thought to be things such as CNS infections and trauma.
During childhood, well-defined epilepsy syndromes are generally seen.
During adolescence and adulthood, the causes are more likely to be secondary to any CNS lesion. Further, idiopathic epilepsy is less common. Other causes associated with these age groups are stress, trauma, CNS infections, brain tumors, illicit drug use and alcohol withdrawal.
In older adults, cerebrovascular disease is a very common cause. Other causes are CNS tumors, head trauma, and other degenerative diseases that are common in the older age group, such as dementia.When investigating the causes of seizures, it is important to understand physiological conditions that may predispose the individual to a seizure occurrence. Several clinical and experimental data have implicated the failure of blood–brain barrier (BBB) function in triggering chronic or acute seizures, some studies implicate the interactions between a common blood protein—albumin and astrocytes. These findings suggest that acute seizures are a predictable consequence of disruption of the BBB by either artificial or inflammatory mechanisms. In addition, expression of drug resistance molecules and transporters at the BBB are a significant mechanism of resistance to commonly used anti-epileptic drugs.
Few medical conditions have carried the mystique or generated as much controversy as epilepsy. Coping with societal challenges can be the most difficult part of having epilepsy. November is Epilepsy Month, a time to promote awareness of epilepsy, the third most common neurological disorder, affecting approximately 2.5 million Americans. It has been estimated that 10% of the American population will experience a seizure in their lifetime. Every year there are nearly 181 thousand newly diagnosed epilepsy cases in the United States, and over 45 thousand of these are children under 15 years of age.
Epilepsy is defined as the recurrence of two or more unprovoked seizures requiring long-term treatment with anti-epileptic (AE) medication.
New cases of epilepsy are most common among children, especially during the first year of life. Another peak of new cases occurs in the elderly. Treatment is usually a single medication. Important considerations when introducing therapy include age, gender, concomitant medical illnesses and medications. For example, elderly patients and pregnant women require modified treatments.
Up to 30% of all epilepsy cases can not be controlled with AE medications. Diagnosis and treatment of these patients is usually referred to a specialized epilepsy center, like the California Pacific Epilepsy Center, located at California Pacific Medical Center. The epilepsy team reviews all hospital findings to determine the area in the brain where the seizures originate. If the focus of the seizures cannot be determined, the patient may be a candidate for inpatient surgical evaluation.
The California Pacific Epilepsy Center provides patients with comprehensive care for epilepsy and epilepsy-related problems using state-of-the-art technology and resources to perform diagnostic procedures, medical management and surgical care for adolescents and adults. With new medical and surgical treatments, the California Pacific Epilepsy Center offers hope to patients who do not respond to standard medication and suffer the disabling stigma attached to epilepsy. The Epilepsy Center balances treatment of epilepsy symptoms and assistance with psychological, educational and vocational issues encountered by epilepsy patients and their families. Read more about the California Pacific Epilepsy Program. FIND A DOCTOR
POTENTIAL CURE
The ‘ketogenic diet’ is a high-fat, adequate-protein, low-carbohydrate diet that in medicine is used primarily to treat difficult-to-control (refractory) epilepsy in children. The diet mimics aspects of starvation by forcing the body to burn fats rather than carbohydrates. Normally, the carbohydrates contained in food are converted into glucose, which is then transported around the body and is particularly important in fuelling brain function. However, if there is very little carbohydrate in the diet, the liver converts fat into fatty acids and ketone bodies. The ketone bodies pass into the brain and replace glucose as an energy source. An elevated level of ketone bodies in the blood, a state known as ketosis, leads to a reduction in the frequency of epileptic seizures.
The original therapeutic diet for pediatric epilepsy provides just enough protein for body growth and repair, and sufficient calories to maintain the correct weight for age and height. This classic ketogenic diet contains a 4:1 ratio by weight of fat to combined protein and carbohydrate. This is achieved by excluding high-carbohydrate foods such as starchy fruits and vegetables, bread, pasta, grains and sugar, while increasing the consumption of foods high in fat such as cream and butter.
Most dietary fat is made of molecules called long-chain triglycerides (LCTs). However, medium-chain triglycerides (MCTs)—made from fatty acids with shorter carbon chains than LCTs—are more ketogenic. A variant of the classic diet known as the MCT ketogenic diet uses a form of coconut oil, which is rich in MCTs, to provide around half the calories. As less overall fat is needed in this variant of the diet, a greater proportion of carbohydrate and protein can be consumed, allowing a greater variety of food choices.
The classic therapeutic ketogenic diet was developed for treatment of pediatric epilepsy in the 1920s and was widely used into the next decade, but its popularity waned with the introduction of effective anticonvulsant drugs. In the mid 1990s, Hollywood producer Jim Abrahams, whose son’s severe epilepsy was effectively controlled by the diet, created the Charlie Foundation to promote it. Publicity included an appearance on NBC’s Dateline programme and …First Do No Harm (1997), a made-for-television film starring Meryl Streep. The foundation sponsored a multicentre research study, the results of which—announced in 1996—marked the beginning of renewed scientific interest in the diet.
The diet is effective in half of the patients who try it, and very effective in one third of patients.[4] In 2008, a randomised controlled trial showed a clear benefit for treating refractory epilepsy in children with the ketogenic diet. A treatment of 6 to 24 months duration frequently results in a ≥ 90% decrease or elimination of seizures.
There is some evidence that adults with epilepsy may benefit from the diet, and that a less strict regime, such as a modified Atkins diet, is similarly effective.
Clinical trials and studies in animal models suggest that ketogenic diets provide neuroprotective and disease-modifying benefits for a number of adult neuro-degenerative disorders. As of 2008, research in this area is regarded as having provided insufficient data to produce clear practice parameters for clinical protocols.
Use Epilepsy Month to take good care of yourself.
Do something very simple for yourself like getting 8 hours of sleep, or try a new medication to get better control of your seizures. You might even attend a meeting of the support group that you have been conflicted about joining.
Epilepsy Month’s goal is to increase the public’s awareness about epilepsy. Everyone with epilepsy can easily participate in building awareness of epilepsy just by sharing his or her story. Tell someone in your school, workplace, or house of worship that you have epilepsy and share something about epilepsy that is unique to you. The general public overestimates the impact epilepsy has on lifestyle. By sharing your story you can open the mind of one person and spread the reality of epilepsy by word of mouth. Watch those misconceptions fall like dominos!
However you choose to participate, don’t let Epilepsy Month pass you by!
Epilepsy Awareness Month – November
November 11, 2012 by